Hospital Design from the Nurse’s Perspective

With their new bed tower at Pineville, North Carolina, Atrium Healthcare asked us to help them finalize new patient room standards as they moved to an open core concept. This change to nursing operation as well as the built environment would inform and streamline the process not only at Pineville, but on the next five projects coming on board adding approximately 1000 new beds to the system.
The Way it Was
This change to nursing concepts revolves around the traditional nurses’ station. Historically one centralized station is where the nursing staff congregated to gather supplies, talk with doctors, manage caseloads. When a patient needed a nurse, they used their call button to summon help, and the nurse would take off down what is known as the “racetrack” corridor, with patient rooms down one side of an eight-foot wide hallway, with equipment and supplies on the other side. Nurses all worked from centralized stations in the middle of these racetrack corridors.

A New Nursing Model
The new open core concept doubles the hallway size to 16 feet wide, and places nurses’ stations within the corridor, one for every four rooms on either side of the hallway. In the new open core model, the nurse doesn’t have to leave the unit or go “off-stage” as frequently as the old model, as all services are available within reach of their assigned pods. Everything from medications and supplies, to processing of soiled linens, disposable waste, and nourishment stations are all within a pod, so the nurse can stay within arm’s reach of her patients throughout most of her shift.
Nurses are more efficient and available, eliminating wasted steps traveling up and down the corridor to retrieve supplies. They remain at bedside more than in the previous design. And patients feel supported and cared for with nurses more readily accessible and visible through the doorway window if they have a need. Each of the pod nursing stations are Y-shaped, where nurses can sit or stand. Even at the sitting station they have visual access to all four patients.
Change is always difficult, especially in areas where we work and know how our spaces work. And this change was no different for the nurses, practitioners, and doctors who had to adapt to this new model. Since the new concept at Pineville was an addition to an existing facility, there was some resistance from staff coming over from the older units into the new bed tower.
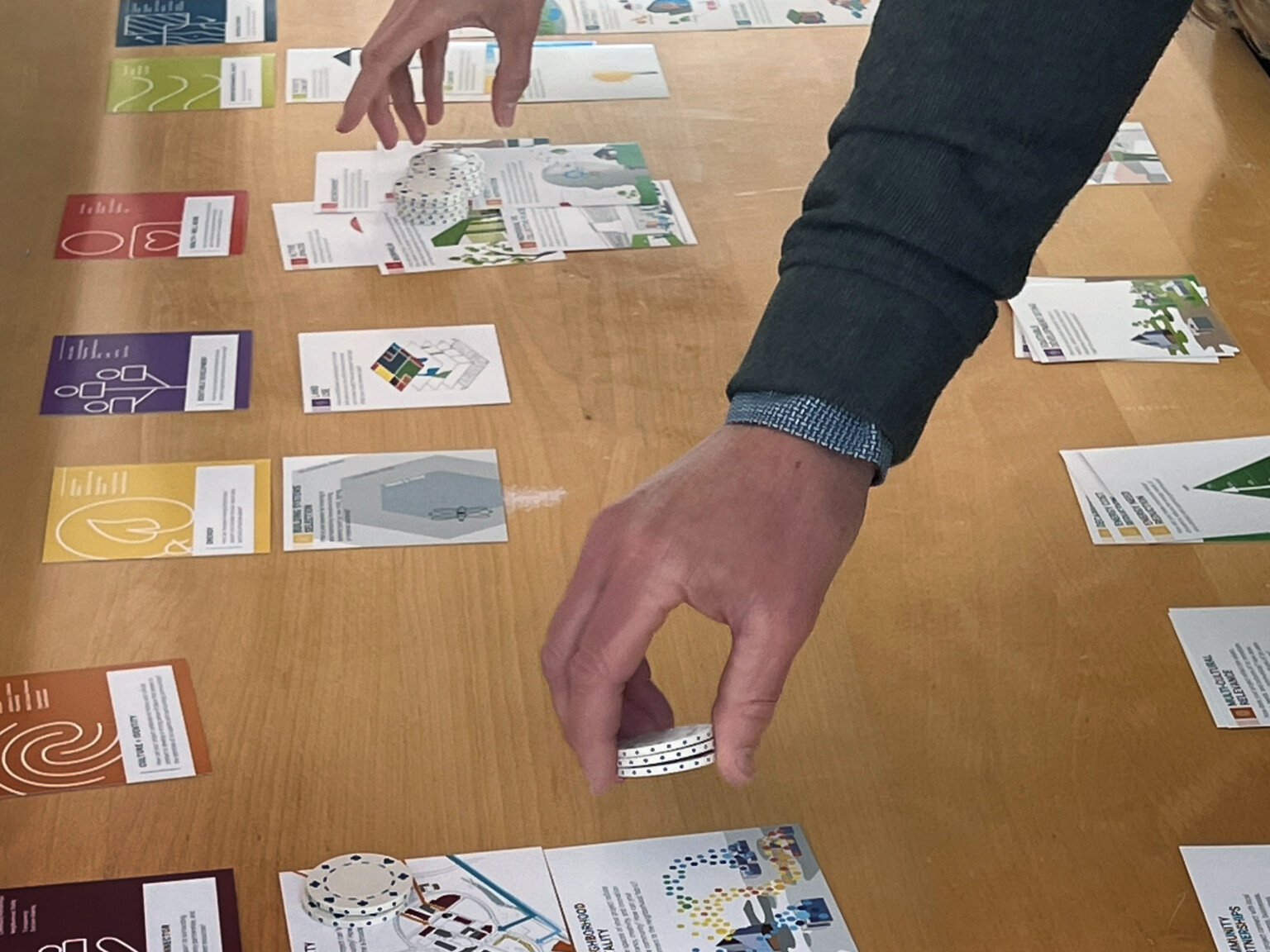
The design team worked with Atrium to get buy-in from staff early in design using mock-up patient rooms and nursing stations. This allowed the staff to get a feel for the spaces, making suggestions to improve efficiencies, and answer the basic questions of “How do you take care of a patient? What are the steps that you need to care for a patient? How would you do it if you weren’t at Pineville?” Then, later after design was complete, medical staff went through three to four weeks of training in the space with the new technology, both for the experienced nurses as well as new staff.
Technology was also a challenge due to designing the patient rooms to be adaptable for other uses, including potential as medical/surgical rooms that can go up in acuity levels. They also asked that the rooms be adaptable into Intensive Care Unit rooms which means more flexibility in the design, different types of cabling for future use. When rooms become ICU rooms, they implement telehealth elements, with a video camera available in every room for attending physicians or specialists to call in to consult with the patient via a secondary patient monitor so the doctor can be visible to the patient.

Construction Efficiencies
As positive as this model is in improving staff efficiencies and levels of patient care, there is another reason why this is an important adjustment to hospital design. Although the corridor size is doubled, the support spaces and “unused” square footage of the old corridors in fact end up saving square footage in the final design which relates directly to cutting cost of construction. The original bed tower floor plate was approximately 33,000 SF, compared to the new floorplate at just over 31,000 SF. That’s a reduction of 5.8% in square footage.
This concept also speeds the delivery of the building by using prefabrication elements such as above-ceiling multi-trade racks, and engineering systems. Due to the wider corridors and more space above ceiling, this eliminated the need to take these systems into patient rooms. In addition to prefabricated engineering systems, the patient room headwall and footwall as well as the toilet rooms were also manufactured off site which sped up time of construction with a higher level of finish design.
Finally, the exterior skin of the tower was pre-manufactured offsite, and delivered ready to install. The old methods of building and constructing facades on-site could take up to 11 months to dry in. With systems being pre-manufactured off site, they arrive ready to install and were completed in 11 weeks for complete dry in, saving time and budget.
The changes to the nursing model reach far beyond improving healthcare methods. It also can improve job satisfaction for highly efficient medical staff, as well as improving timeline, budgets, and quality of design and construction delivery of healthcare facilities in general.